Anatomy of the urinary system and distribution of disease across its organs are presented on the ‘Overview’ page. It is recommended to read the ‘Overview’ page first.
Over one hundred years ago, Cullen TS described the first published case of ureter disease in “Adenomyosis of the rectovaginal septum” (Johns Hopkins Hospital Bulletin, 1917). Very slow advances in the identification and treatment have evolved in this time period. Awareness that endometriosis of the ureter is an area which deserves far greater attention is clears in areas of education, screening and interventions. In addition to the need for improved communication and crossover boundaries of gynecologists and urologists is needed.
Although the frequency of ureter(s) disease is significantly less than the bladder, delayed diagnosis and inadequate treatment can result in serious, irreversible damage and potential kidney loss. In fact, aggressive disease of both ureters has led to loss of life. (1) The loss of life is an extreme, and based upon a lack of publications, is a rare occurrence. However, various degrees of compromised renal function among those with ureter disease is a reality. By the time ureter disease is identified, at least 30-43% of cases will have lost 25-50% of functional kidney tissue. (2-5) A large retrospective review which analyzed the data from numerous studies with reports of at least 5 cases each, found nearly one half (48.3%) of patients who underwent laparoscopy had some degree of preoperative kidney nephrosis (death of a portion of renal tissue). (6)
“…subclinical disease is probably underestimated due to being easily missed even upon surgical inspection, which means the prevalence is actually higher than assumed” – Maccagnano C et al (2013) (2)
The probability of Urinary System Endometriosis among persons with deep infiltrating endometriosis (DIE) justifies diligence in monitoring these persons. Specific characteristics of deep infiltrating endometriosis, ie. anatomical location and size, identify those with high risk of ureter disease. These include lesions of the uterosacral ligaments (3,7,8,) and rectovaginal nodule(s) (3,7,8). Those with RVS lesions > 30mm diameter are 4:1 more likely to have disease of the Ureter. (7,9) Lesions of the digestive system (particularly the rectum and sigmoid colon) also have elevated risk of ureter disease. (8,10)
“Patients with retrocervical endometriosis were found to have a 7-fold greater chance of having urinary tract endometriosis and for patients with endometriosis of the rectum-sigmoid, this chance was 22-fold greater” Westney OL et al. (2000) (10)

How common are lesions of the ureter & bladder in the same person?
Smaller studies frequently report lower rates of 10-25%. (7,11) A large review, which gathered published studies of 700 cases, found a net average of nearly 20%, for concurrent disease. (6)
Where are lesions most frequently located along the ureter?
Distal (lower) 1/3 > Middle 1/3 > Proximal (upper) 1/3. (2)
The distal 1/3 of the ureter travels behind a layer of tissue (peritoneum) and includes its entrance into the bladder.
How often does endometriosis affect the Left, Right and Both Ureters?
Left Ureter > Right Ureter > Bilateral Ureters
A range of ratios, gathered from varied sample sizes are reported. All variations denote disease of the left ureter is more common than the right. Reported ranges of 5:2, 4:1 (2,3,8) and as low as 2.2:1 are documented. (4)
The incidence of disease affecting both ureters among the same person is reported as low as 2.4%. (4) An average range of 10-23% is frequently observed (2,5,6) but as high as 33% of cases referred to specialty centers with higher caseloads of complex disease. (7)
How does Extrinsic Ureter Endo. and Intrinsic Ureter Endo. differ?
Ureter disease can be categorized as ‘extrinsic’ and ‘intrinsic’. As disease progression is variable, it is possible to have both present in the same person. Identification of the degree of invasion toward the lumen of the ureter is crucial for surgical planning and use of appropriate surgical technique(s).
Extrinsic > Intrinsic
Extrinsic endometriosis is far more common than Intrinsic endometriosis. An average of 80%, (range 78-90%) is disease on tissue near the ureter or if directly on the ureter, does not invade into the ureter. Disease that has penetrated through ‘at least’ the muscular wall’ inward to include the lumen of the ureter has been reported with an average of 20% (range 7.3-33%). (4,12,13) Ureteroscopy is able to directly visualize lesions if they have penetrated through all layers into the lumen. (14)
Clement states ‘Endometriosis lesions involving the overlying peritoneum, uterosacral ligament, or ovary resulting in compression of the ureteral wall as well as lesions involving the ureteral mucosa and/or muscularis”…
In case of intrinsic ureteric endometriosis, ectopic endometrial tissue infiltrates directly through the muscularis propria, lamina propria or ureteric lumen.” (3) – Clement PB in Talreha et al
Has anyone ever had endometriosis of the ureter without presence anywhere else in the body?
Yes. (15)
Symptoms of Ureter Disease:
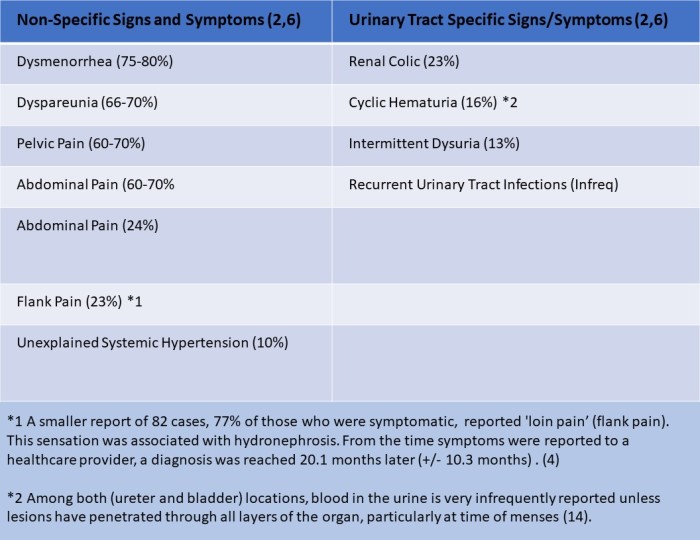
No symptoms occur in 50-75% of those with ureter disease. (2,4,5,7) Those with symptoms (25-50%), symptoms are mostly ‘non-specific’ (vague and difficult to pin-point). A list of symptoms (based upon two studies of 200 and 700 cases) include (2,6):
Differential Diagnosis (2,14):
- Ureteral Carcinoma (primary cancer)
- Metastatic Ureteral Carcinoma (secondary cancer)
- Retropertioneal Lymphadenopathy
- Idiopathic Retroperitoneal Fibrosis
Clinical Assessment and Imaging:
(Note: tests ordered will differ between gynecology and urology. some primary care providers may also request some of these tests during early investigation)
- Bimanual Examination
- Urinalysis (Blood componens; bacteria count; protein levels)
- Blood Panel (assess renal function)
- Transvaginal Ultrasound (TVUS) and Transabdominal US
- MRI (next level of imaging. More expensive)
- CT Scan
- Ureteroscopy and Cystoscopy (explained below)
- Intravenous Pyelogram (IVP)
- Renal Scan
Patient Perspective:
“When it was found by ultrasound, the gynecologist refused it was endometriosis and said it was an infection. Thankfully the urology team wasn’t having it and did the CT Scan which confirmed endometriosis. A cyst was pressing on my ureter…
My urology doctor discussed losing my kidney a few times, and the pressure being placed on my healthy kidney…
I had a kidney stent for years which was changed every 12 months. The endometriosis got a lot worse (which was confirmed by special retrograde imaging). It was then changed every 9 months due to rising pressure making the stent ineffective. If not for the stent, my ureter would have fully closed…
After the stent was removed, a nephrostomy tube was inserted…
The prolonged use of double jj stents altered my bladders function. As a result, I developed urinary retention. I had to learn how to catheterize myself and the concerns of the need for an indwelling catheter to be placed long term.” – Sue (2018)
Medical Management versus Surgical Intervention:
There are current discussions that attempt to identify non-progressive from progressive endometriosis in close proximity or direct contact of the ureters. No factors have been identified yet. The common factor that hysterectomy with removal of both ovaries as a hormonal management approach, without removal of all endometriosis lesions and as much fibrosis as possible, has been demonstrated to be an ineffective treatment method in some cases (16). It is reported that most injury to the ureter is the result of progressive fibrosis. As fibrosis thickens, it contracts and becomes more firm. These properties create progressive compression forces that may result in closure of a ureter’s lumen (passage for urine). Urine is retained in the kidney, leading to enlargement. The presence of two kidneys, like two lungs, is a built-in redundancy that allows a the other kidney to compensate for the ailing kidney. However, this is not an ideal scenario.
“…as ureter obstruction is usually due to fibrosis, lesions rarely respond to medical treatment.” (7) – Knabben L et al. (2014)
Endometriosis of the urinary system requires the skills of both a gynecologist and urologist to identify and removal all disease. The proximity of the reproductive, urinary and digestive organs and probability of at least two of these three systems affected in persons with Deep Infiltrating Endometriosis, necessitates a team of surgeons of their respected expertise to promote best outcomes with the lowest complication rates.
“Given a high risk of silent kidney loss, it is recommended that patients with ureteral involvement by endometriosis are managed by a multidisciplinary team considering urinary and potential extra-urinary localizations of endometriosis (grade C).”(17) – Bolze PA et al. (2015)
Definitions of Procedures*:
Cystectomy (partial): The removal of all or a portion of the urinary bladder.
Cystoscopy: A rigid endoscope for inspecting and passing instruments into the urethra and bladder.
Ureteroscopy: Examination of the interior of a ureter by means of a ureteroscope.
Ureterolysis: A surgical procedure to free a ureter from abnormal adhesions or surrounding tissue (as in retroperitoneal fibrosis)
Ureterectomy: Surgical excision of all or part of a ureter.
Anastamosis (end to end): The union of parts or branches (blood vessles, ureter sections) so as to intercommunicate or interconnect.
Ureteroneocystostomy: Surgical reimplantation of a ureter into the bladder.
(* All definitions may be verified at https://www.merriam-webster.com)
___________________________________________________________________________________________
Current and historical literature have a common theme in regards to contemplating what is/are the ‘best’ surgical approach(s) for different degrees of disease of the ureter. Comparison of literature from 2006 to 2018 shows a movement from more to less aggressive approach to ureter disease with recommendation of ureterolysis unless moderate to severe disease is present. (2,3,11,12) A variety of procedures are available and can considered based upon the:
- Depth of disease penetration into the ureter tissue layers
- Length of the ureter involved (ie > or < 3 cm)
- Location of disease (ie. above or below the Iliac vessels)
- Presence and degree of hydronephrosis.
The three procedures, in order of least to most aggressive approach include Ureterolysis, Ureterectomy and Ureteroneocystostomy. All three procedures are performed through laparoscopy (a laparotomy may be needed in some instances). If ureter stents are placed, entranced through the urethra, bladder and into the ureter is performed prior to the procedure.
Ureterolysis the least invasive procedure. (5) Most often, stents are placed within the ureter (by entering the bladder and guided up into the ureter. This provides a solid edge for the surgeon to free the ureter up from fibrosis. A surgeon has different options for best tool. There is not ‘cutting into’ the ureter with this technique. What cases are considered appropriate for this technique? Based upon collective publications gathered over time, there has been a gradual shift toward ureterolysis for a greater range of presentations.
Over recent years a more conservative approach to ureter disease with ureterectomy and ureteroneocystostomy reserved for more involved disease and greater degree of hydronephrosis. A (2012) triple case study and literature review article identified Grade 2 hydronephrosis to move from ureterolysis to ureterectomy for best long-term outcomes. (3) It is important to realize each surgeon has flexibility to determine what is the ‘best fit’ for each patient’s need, and ‘best approaches’ and ‘best outcomes’ for their clinic for specific presentations. Based upon published experiences gathered over time…
“The choice between ureterolysis and segmental resection in the treatment of ureteral endometriosis remains controversial” (8) -Rozsynai, F et al. (2011)
“…it remains controversial whether ureterolysis is sufficient or whether more invasive methods such as ureterectomy are necessary to prevent recurrence ” (7) – Knabben, L et al. (2014)
Ureterocystectostomy This procedure is recommended for lesions near the end of the ureter as it enters the bladder, or if lesions on the bladder occur within 2 cm of where the ureter-to-bladder merge. (R)
Where does this leave us?
It is clear that the academic institutes of medicine need to improve didactic information regarding endometriosis in medical school. It is clear that education, screening and assessment practices should overlap and yes, be redundant between gynecology and urology to ensure disease is not missed early. This redundancy is essential as is the necessity of direct communication between specialists, without the patient acting as messenger between the disciplines. Last, as with all areas of endometriosis, funding has been limited, urgency has been absent and lack of awareness of the true extent of body-wide disease has led to a snowball in healthcare costs and loss of life’s quality and contribution of many women with this disease.
“Because the prevalence of urinary tract endometriosis is relatively low (perceived), the only way to assess effective treatment is through a large randomized study involving surgical teams worldwide, skilled in both radical and conservative approaches, where outcomes are recorded, not only in terms of recurrence rates but also risk of postoperative complications”(8) – Ruzsnyai, F et al. (2011)
Ureter Endometriosis Citation List
Looking for a support and education group?
Extrapelvic Not Rare Endometriosis Education and Discussion Group


All Rights Reserved © 2018 Wendy Bingham, DPT. Extrapelvic Not Rare