We are Trish
Since the time endometriosis was recognized outside the reproductive system, we have been know as atypical and rare. Eventually atypical were collectively Extrapelvic Endometriosis.
Initially, endometriosis lesions located outside the internal genitally and support structures were divided into two groups: extragenital and extrapelvic. Still today, a single nomenclature to identify endometriosis lesions based upon location in mutually exclusive categories is lacking. This continues to create confusion and misinterpretation among literature that fails to define locations included/excluded. (ie. dependent upon investigator, academic institutes, geographical region some or all extragenital lesions are considered Pelvic Endometriosis while other investigators, academic institutions and geographical regions considered some or all extragential lesions as Extrapelvic Endometriosis.
Extrapelvic Not Rare adheres to the following definitions of Pelvic and Extrapelvic Endometriosis:
Disease of the reproductive organs and surrounding tissue are referred to as Pelvic Endometriosis. include lesions of the ovary, fallopian tubes, uterus, Pouch of Douglas (Posterior Cul-de-Sac), supportive ligaments (Uterosacral, Broad and Round), pelvic sidewalls and local peritoneum. (Markham, 1997)
Extrapelvic endometriosis (EPE), refers to endometriosis implants found anywhere else in the body (ex. gastointestinal tract, urinary tract, pulmonary system, extremities, skin and central nervous system” (Markham, 1997). As awareness grows, increased interest into research supports the idea Extrapelvic Endometriosis (EPE) is more prevalent among the community than recognized.
Here we are today…
Use of terms like ‘rare’ and ‘atypical’ persist despite accumulating data that disputes this. Use of rare, atypical and similar descriptors create both conscious and unconscious bias among providers. It dissuades investigation into patients complaints, often rapidly dismissing the patient’s experience. To use ‘rare’ or ‘atypical’ when requesting funds for research are not incentives to allocate funds. These terms create additional barrier to integrating extrapelvic disease into the conversation of endometriosis, consequently affecting those who sufferer.
Whether intentional or not, atypical and rare creates a sense of exclusion. A perception that construes; disease in these areas are ‘outliers’. In science, focus is primarily on the norm (mean and median and those within one standard deviation). Conferences and media about endometriosis, nearly always fail to include Extrapelvic disease in the conversation. Nor do most guidelines for care, around the globe and among all healthcare providers, define or declare treatment standards for extrapelvic disease. These exclusions exists across the entire health spectrum but, most alarming, the primary discipline allocated to care for us has significant room for improvement.
Another reason ExtrapelvicNotRare exists; The discrepancy between what physicians know and perceive about the disease and those with live with it, can be equated to the width of the Grand Canyon. As a medical provider AND a person who lives with the disease, it is startling. The reality for many women assumed to be ‘outliers’ and ‘atypical’ are not. They are far closer to the median or mean than perceived by providers.
Yes, prevalence of extrapelvic disease is substantial. Its inclusion among all conversations about endometriosis is needed. Is the prevalence within one, or two standard deviations? Does it matter?
Perception and awareness of endometriosis as a systemic disease, NOT confined to the female reproductive system is needed. Until we recognize the true systemic nature of the disease, old perceptions will hinder progress to treat those with this disease with appropriate multidisciplinary care. Lets begin.
An estimated 20% (2), and as high as 37% (1), of those who suffer with endometriosis have extrapelvic disease. Lets use the conservative estimate that 1:5 persons (20%) with endometriosis have extra-pelvic disease.

If we gather the persons with extrapelvic disease (again, we use the conservative estimate of 1:5 or 20%), what is the probability, per person for location of disease by system involved? Let’s look at the probability pie graph:
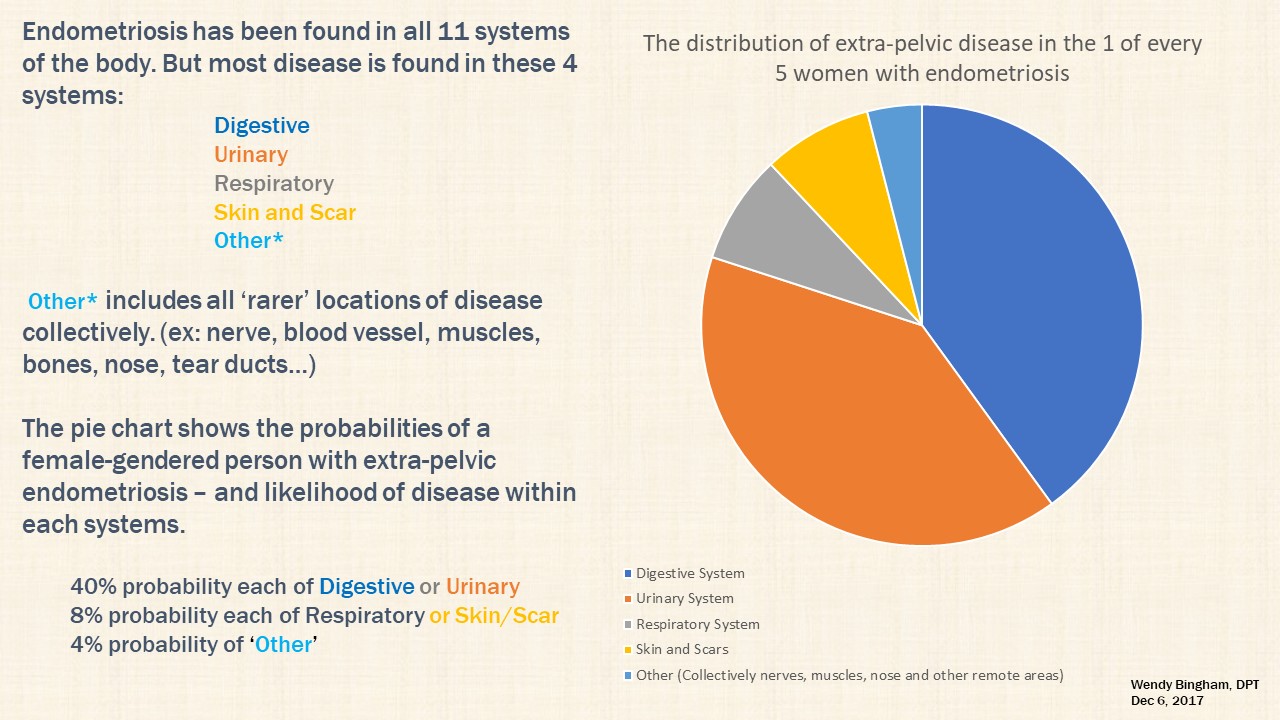
As demonstrated in the pie chart above, the digestive (gastrointestinal system and accessory organs) and urinary/excretory systems are involved most often, followed by the respiratory and integumentary systems (cutaneous/skin). Less frequent, the circulatory, endocrine, lymphatic, muscular and skeletal systems are involved (1). (Note: the liver and gallbladder are adjunctive organs of the digestive system organs. No prevalence estimates are given for these organs and thus excluded from the pie chart above.)
Traditionally endometriosis has been considered a disease of the female reproductive system. Endometriosis is, in-fact, a disease which is multi-organ, multi-system, chronic systemic inflammatory disease; disease with body-wide potential. As such, there is a need to bring awareness, education and implement changes for how this disease is approached across the entire healthcare spectrum.
The reality: endometriosis requires a multidisciplinary approach. The presence of extrapelvic lesions necessitates greater development of advanced education and training for this disease. This is needed across all surgical disciplines. The medical education and collaboration should resemble that used for diabetes mellitus. Family Practitioners, Pediatricians, Internists, Gynecologists Nurse Practitioners, allied health professionals etc. should be included with the spectrum of surgical specialists. Early identification and ‘best’ treatment is vital for minimal long-term damage. ‘Best treatment’ may involve recognition of a providers limitations and appropriate referral to a endometriosis excision surgeon with advanced clinical, didactic and surgical training.
Endometriosis impacts every aspect of a person’s life. Thus, patient-centered treatment is vital. The perception, experience, dismissal and delayed diagnosis of sufferers, as a result of poor awareness, education and limited treatment options offered by providers, are integrated into the website content. Integration of the patient experience here provides opportunity to better identify problems and consider solutions. Those who receive care by a skilled, experienced excision surgeons (and their teams) most often learn through online support and education groups created by sufferers, for sufferers. These groups present up-to-date information about the disease which the general healthcare providers, this includes Gynecologists have NOT acquired in medical school curricula or professional continuing medical education.
Something is very wrong when the endometriosis community of sufferers are more knowledgeable in best treatment options and advanced understanding about the disease, the system is broken. The only correct way to fix the system is to first integrate advocates and those with the disease to provide equal input for progress to be made.

Originally Published: July 10th, 2018
Last Updated: June 1st, 2020